
Corneal Transplant Surgery
Corneal Surgery
Dr. Neil B. Griffin’s practice is somewhat unique. He was fortunate to have an early concentration in his medical career on cornea and external disease. As of today Dr. Griffin has performed over 2000 corneal transplants. His early experience with lamellar transplant surgery put him in position to help introduce some major advancements in cornea transplant surgery.
“Cornea practice is very rewarding because you can help patients who are often experiencing pain or facing serious vision threatening conditions.” -Dr. Griffin
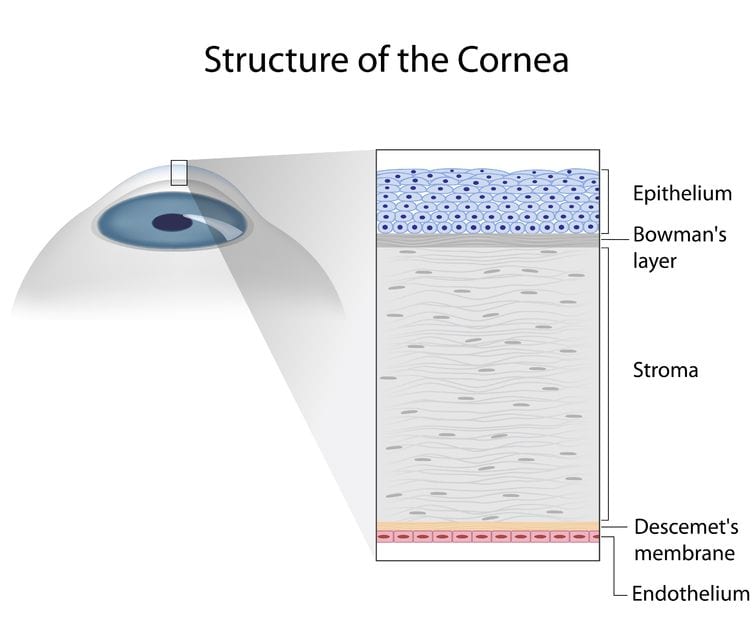
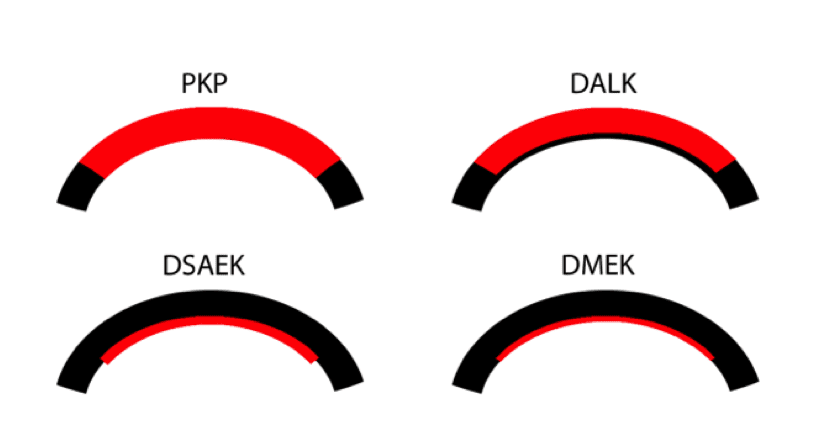
To simplify, the cornea has three main layers; the surface epithelial layer, the wall or stroma, and the endothelial cell layer on the inside. Consider the endothelium as its basement membrane, Descemet’s, as one layer. Patients can have a problem with stroma, endothelium or both.
The stroma provides the strength and shape of the cornea. It determines focus for the eye. It can be scarred from trauma or disease.
The endothelial cell layer keeps the stoma dehydrated and clear. If you lose too many endothelial cells, your stroma swells and is cloudy. With new endothelial cells, the stroma returns to normal
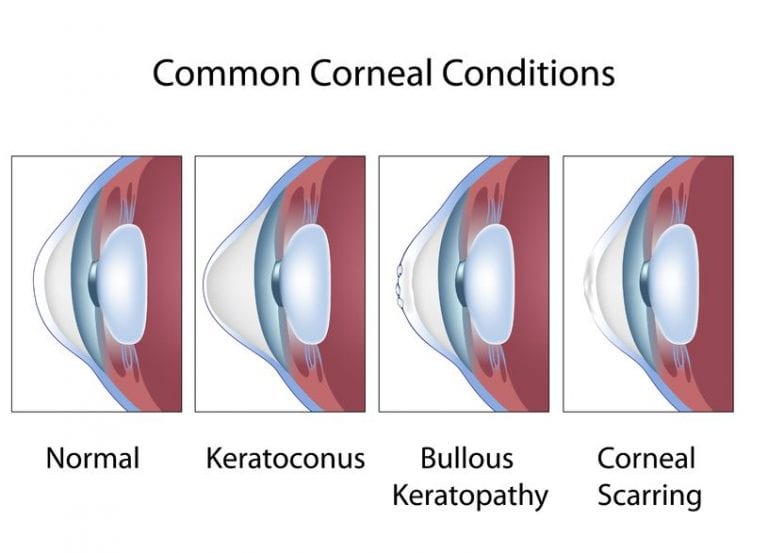
Keratoconus is a condition in young people where the stroma is thin and cannot hold a good shape to allow good focus. The endothelium is normal but the stromal wall may need to be replaced.
Keratoplasty PK
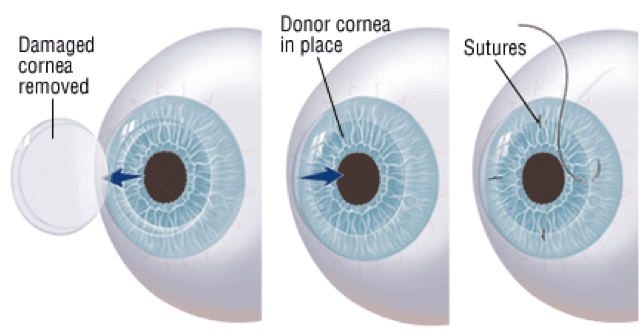
In the past there was only one corneal transplant procedure, penetrating keratoplasty PK, a full thickness cornea transplant. The stroma and endothelium are both replaced. Sight is restored but recovery is slow. It sometimes takes over a year to restore good focus from the hand sewn cornea wall. Penetrating keratoplasty is still required for full thickness problems, but advances in lamellar (layered) techniques allow us to transplant the layer involved, sparing normal layers. This has major advantages for patients.
Deep Anterior Lamellar Keratoplasty
Dr. Griffin has performed lamellar keratoplasty for his entire career. Dr. John Goosey, who provided the other cornea fellowship at Houston Eye, was a pioneer in Deep Anterior Lamellar Keratoplasty (DALK) the first successful lamellar technique.
Here we save the normal endothelium and replace the thin stroma. The most common indication for DALK is in young patients with keratoconus. They still require a hand sewn stroma and a long recovery, but they keep their normal endothelium. This is important because the most common reason for full thickness transplants to fail is due to loss of the transplant’s endothelial cells over time. If you can save the patient’s normal endothelium they are less likely to need repeat transplants.
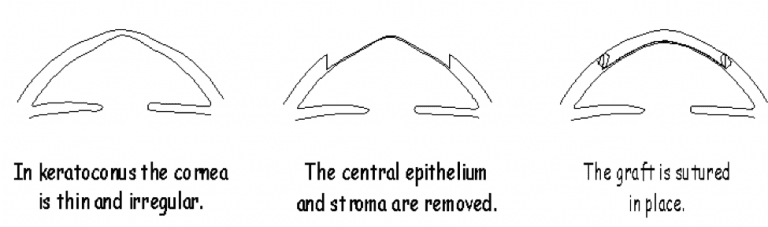
Dr. Griffin has been performing DALK for young keratoconus patients since 1994. “There were only a handful of DALK surgeons at that time and the numbers were slow to increase. The Europeans are way ahead of US surgeons in DALK even today. DALK required more time in the operating room. Most surgeons were easily convinced that PK was just as good for their keratoconus patients,” Says, Dr. Griffin.
In Dr. Griffin’s career the most important cornea surgical advancement took place in 2003 when Dr. Garrett Melles described what was later named Descemet’s Stripping Endothelial keratoplasty (DSEK or DSAEK). Dr. Griffin has trained with Dr. Melles in the Netherlands and Dr. Griffin is one of the first surgeons in the US to provide the surgery.
With DSEK or DSAEK a patient’s abnormal endothelium with its Descemet’s membrane is stripped from the inside of their normal stroma. The thin donor graft is then attached to the inside of the patient’s cornea.
The opposite of DALK, DSAEK is indicated for patients who have a normal stroma but a problem with endothelial cells. The procedure is sutureless and patients recover good vision in a few months. Endothelial failure is responsible for approximately 85% of transplants, so this is truly a major breakthrough.
The latest advance, also the work of Melles, is Descemet’s Membrane Endothelial Keratoplasty. In DSAEK, the thin donor graft consist of the endothelial cells, their Descemet’s membrane and a little bit of the attached stroma. The thin stroma acts as a carrier for the endothelial cells and makes it easier to transplant. The DMEK donor is only cells and Descemet’s membrane. The vision and the incidence of graft reaction is better with DMEK. Dr. Griffin has performed DMEK for approximately four years. It is now Dr. Griffin’s first choice procedure for endothelial failure. He was first in the state to add DMEK and there are only a handful of DMEK surgeons in the Carolinas today.
